fatty liver diet plan pdf
Understanding Fatty Liver Disease
This condition, also known as hepatic steatosis, results from excessive fat accumulation in the liver, severely impairing its vital functions․ It frequently co-exists with conditions like obesity and diabetes, leading to serious health complications and damage․
Definition of Hepatic Steatosis
Hepatic steatosis, more commonly recognized as fatty liver disease, is a significant medical condition characterized by the abnormal and excessive accumulation of fat within the liver cells․ This accumulation goes beyond the normal amount of fat typically found in the liver, leading to a pathological state․ When liver cells store an abundance of fat, it begins to impair the organ’s ability to perform its myriad crucial functions efficiently․ The liver, being one of the largest internal organs, acts as a metabolic factory, processing virtually everything we consume after digestion․ Therefore, any compromise to its function due to fat overload can have widespread implications for overall health․ This condition is not merely a benign presence of fat; rather, it’s a precursor to or an indicator of potential liver damage and serious health complications․ Understanding this fundamental definition is the first step in addressing and managing the disease effectively, often through targeted dietary and lifestyle interventions․ The presence of this excessive fat directly hinders the liver’s capacity to filter toxins and process nutrients, creating dangerous health problems․

Impact of Fat Accumulation on Liver Function
The excessive accumulation of fat within the liver cells profoundly impairs the organ’s critical functions․ When fat infiltrates liver tissue, it disrupts the intricate cellular machinery responsible for metabolism, detoxification, and nutrient processing․ The liver, often referred to as the body’s metabolic factory, is tasked with a myriad of vital processes, including filtering toxins from the bloodstream, synthesizing proteins, producing bile for digestion, and regulating blood sugar․ Fatty liver disease directly compromises these capabilities․ The presence of too much fat hinders the liver’s efficiency, making it less effective at performing its essential duties․ This impairment can lead to a cascade of health problems, as the body relies heavily on a properly functioning liver for overall homeostasis․ The disrupted cellular environment can also lead to inflammation and scarring over time, potentially progressing to more severe liver conditions like fibrosis or cirrhosis․ Thus, the impact extends beyond mere fat storage, creating dangerous health problems that affect the body’s ability to maintain health and process ingested substances․
Causes: Excessive Fat Accumulation
Excessive fat accumulation within the liver tissue is the direct cause of fatty liver disease, a condition that significantly compromises liver function․ This detrimental buildup occurs when the body stores more fat than the liver can efficiently process or export, leading to a surplus that infiltrates hepatic cells․ One of the primary drivers behind this is obesity․ Individuals carrying excess body weight are at a substantially higher risk, as their metabolic systems are often overwhelmed by a surplus of calories, leading to increased fat synthesis and storage in various organs, including the liver․
Another significant contributing factor is type 2 diabetes mellitus․ The metabolic dysregulation characteristic of diabetes, particularly insulin resistance, can promote increased fat delivery to the liver and impair its ability to clear existing fat, thus exacerbating accumulation․ Furthermore, certain consumption patterns, such as diets high in refined carbohydrates and unhealthy fats, directly fuel this excessive fat storage․ This continuous influx of lipids, coupled with impaired metabolic regulation and inflammation, creates an environment where liver cells become engorged with fat, leading to the development of this serious health condition and its associated health problems․
Associated Conditions: Obesity and Diabetes
Fatty liver disease is rarely an isolated diagnosis, frequently presenting alongside other chronic conditions, primarily obesity and type 2 diabetes mellitus․ This strong link highlights a shared metabolic dysfunction․ Individuals with obesity, due to excessive body fat, face a significantly elevated risk of developing hepatic steatosis․ This risk stems from systemic inflammation and insulin resistance often associated with obesity, which actively promotes increased fat storage in the liver․

Furthermore, type 2 diabetes is a powerful predictor for fatty liver disease․ Impaired glucose metabolism and chronic high blood sugar levels in diabetic patients often lead to an amplified influx of fatty acids to the liver․ Simultaneously, the liver’s capacity to efficiently process and export existing fat is compromised, resulting in harmful accumulation․ Healthcare providers commonly observe patients with fatty liver are already managing one or both of these prevalent metabolic disorders, making their comprehensive management crucial for liver health․
Dietary Foundations for Liver Health
Dietary changes are a critical part of managing fatty liver disease, directly impacting liver health․ Adopting a Mediterranean diet approach and eating regular, small, frequent meals are foundational strategies that significantly aid in managing this condition․
Dietary Changes as Critical Management
For individuals grappling with fatty liver disease, enacting profound dietary changes stands as an absolutely critical and indispensable component of effective management strategies․ Given that fatty liver, or hepatic steatosis, involves excessive fat accumulation impairing liver function, what we consume holds immense power over the organ’s health and recovery․ The liver, acting as the body’s central metabolic factory, processes every substance ingested, meaning nutrition directly dictates its ability to perform myriad essential functions efficiently․ Therefore, strategic modifications to eating habits are not just beneficial but foundational to mitigating further damage, reducing inflammation, and potentially reversing the progression of the condition․ This proactive shift in diet is paramount for preventing serious health complications associated with compromised liver function; By consciously choosing foods that support liver detoxification and regeneration while avoiding detrimental substances, patients can directly influence their prognosis․ These targeted dietary interventions represent the primary and most impactful therapeutic avenue, offering a direct pathway to restoring liver vitality and improving overall systemic health, thus underscoring their critical role in comprehensive disease management․
Strategic Food Choices for Health
Making strategic food choices is fundamental for individuals dedicated to managing or reversing the progression of fatty liver disease․ The foods we ingest directly and profoundly influence the liver’s intricate ability to detoxify the body, efficiently metabolize fats, and undertake crucial cellular regeneration processes․ Prioritizing nutrient-dense, wholesome foods actively supports optimal liver function and plays a pivotal role in helping to reduce the excessive fat accumulation characteristic of hepatic steatosis․ This endeavor involves a conscious effort to select ingredients rich in essential vitamins, minerals, and antioxidants, which are vital for liver repair and overall metabolic health․ Equally important is the deliberate avoidance of foods widely known to exacerbate liver stress and inflammation․ This strategic approach demands an understanding of how different food groups affect the liver’s workload and its inflammatory responses․ Ultimately, the goal is to construct a dietary framework built around items that actively promote a healthy internal environment․ Such a framework significantly facilitates the liver’s recovery, preventing further cellular damage․ These informed choices empower the body’s largest internal organ to filter toxins more efficiently and perform its myriad functions without undue strain, thereby forming a cornerstone of any effective therapeutic regimen for robust liver health․
Following a Mediterranean Diet Approach
Embracing a Mediterranean diet approach is a highly recommended strategy for individuals managing fatty liver disease, as suggested by experts like “The Liver Doc․” This dietary pattern is renowned for its emphasis on whole, unprocessed foods that actively support liver health and overall well-being․ It prioritizes the consumption of fresh fruits and vegetables, which are rich in antioxidants and anti-inflammatory compounds crucial for combating liver damage․ Extra virgin olive oil, a cornerstone of this diet, provides healthy monounsaturated fats that can help reduce liver fat․
Furthermore, the Mediterranean diet encourages abundant intake of whole grains, legumes, nuts, and seeds, offering fiber and essential nutrients that aid digestion and metabolic function․ Protein sources primarily include fish and lean poultry, with red meat consumed sparingly․ This emphasis on nutrient-dense foods, coupled with a reduced intake of processed items, refined sugars, and unhealthy fats, helps to mitigate inflammation and improve insulin sensitivity, two factors critical in the progression of fatty liver․ Adopting this eating style provides a sustainable and delicious framework for significant improvements in liver function and a healthier lifestyle․
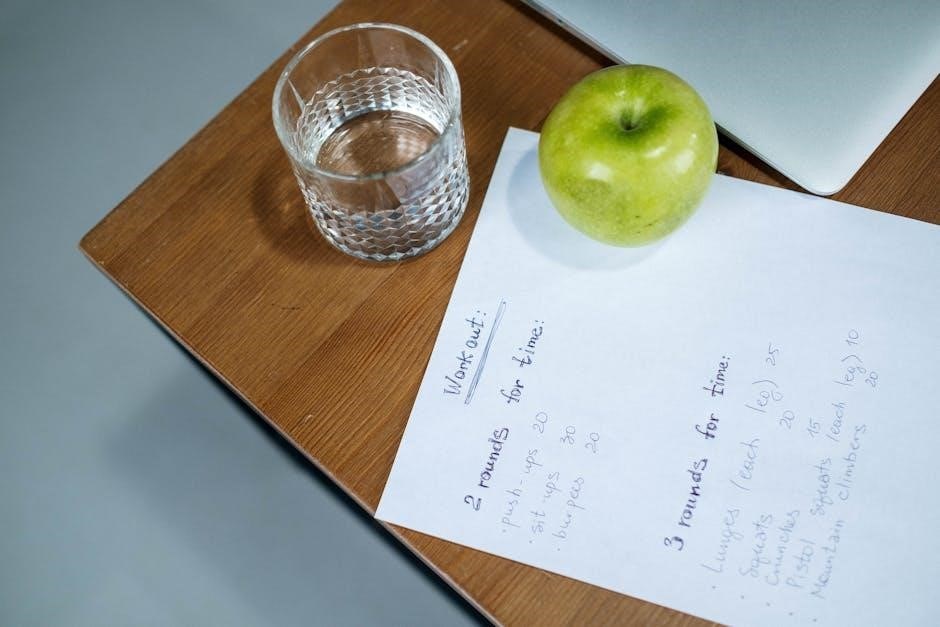
Eating Regular, Small, Frequent Meals
Adopting a strategy of eating regular, small, frequent meals throughout the day is a cornerstone for effective fatty liver management․ This approach is vital for stabilizing blood sugar levels, thereby preventing the dramatic fluctuations that can impose additional stress on the liver and exacerbate fat accumulation․ Instead of overwhelming the liver with large, infrequent meals that demand significant metabolic effort, distributing food intake into smaller portions allows for a more consistent and manageable workload for this crucial organ․
This dietary pattern ensures a steady supply of energy and essential nutrients, optimizing the body’s metabolic processes․ It specifically helps in obtaining sufficient calories and vital nutrients, including protein from sources such as lean meat, eggs, and beans, which are crucial for liver repair and overall bodily function․ By avoiding prolonged periods of fasting followed by overeating, individuals can significantly reduce the likelihood of excessive fat storage in the liver․ Furthermore, frequent smaller meals can effectively aid in appetite control and prevent overeating, which is highly beneficial for weight management, a key factor in mitigating fatty liver progression․ This consistent nutrient intake profoundly supports the liver’s ability to perform its myriad functions efficiently․

Recommended Foods and Preparation
Emphasize whole grains, beans, eggs, fish, and lean chicken․ Incorporate diverse colors into meals for nutrient variety․ Making your own seasonings helps avoid unwanted additives, supporting healthier preparation methods for beneficial eating․
Emphasis on Whole Grains and Beans
Whole grains and beans form a cornerstone of a therapeutic diet aimed at managing fatty liver disease․ Their inclusion is paramount due to their rich nutritional profiles and profound benefits for metabolic health․ Whole grains, such as oats, brown rice, quinoa, and whole wheat, are packed with dietary fiber․ This fiber is crucial for regulating blood sugar levels, preventing the sharp spikes that can contribute to increased fat storage in the liver․ Moreover, the sustained energy release from complex carbohydrates in whole grains helps maintain satiety, potentially reducing overall caloric intake and supporting weight management, a critical factor in combating hepatic steatosis․
Similarly, beans and legumes—including lentils, chickpeas, black beans, and kidney beans—are invaluable․ They offer a potent combination of plant-based protein and soluble fiber․ This dual benefit assists in blood glucose control and promotes a healthy digestive system․ The fiber in beans also contributes to a feeling of fullness, aiding in appetite regulation․ By providing essential nutrients and supporting stable blood sugar and cholesterol levels, whole grains and beans collectively work to reduce inflammation and oxidative stress within the liver, fostering an environment conducive to healing and improved function․ Their regular consumption is a strategic dietary choice to combat fat accumulation effectively․

Protein from Eggs, Fish, and Lean Chicken
Incorporating high-quality, lean protein sources is essential for a diet plan aimed at managing fatty liver disease․ Eggs are an excellent choice, providing complete protein and vital nutrients like choline, which plays a crucial role in fat metabolism and liver detoxification․ Their versatility makes them easy to include in various meals without adding excessive unhealthy fats․
Fish, particularly fatty fish like salmon, mackerel, and sardines, are highly recommended․ These provide not only lean protein but also abundant omega-3 fatty acids․ Omega-3s are well-known for their anti-inflammatory properties, which can help reduce inflammation in the liver and improve overall liver health․ Leaner fish options such as cod or tilapia also offer beneficial protein without significant fat content․
Lean chicken, consumed in small amounts and prepared without skin or excessive oils, serves as another valuable protein source․ It provides essential amino acids needed for liver repair and regeneration without contributing to unhealthy fat accumulation․ Prioritizing these protein options over red meats or processed alternatives supports muscle maintenance, promotes satiety, and aids in the liver’s recovery, making them critical components of a liver-friendly eating strategy․

Incorporating Color in Meals
A visually appealing plate, rich with a spectrum of colors, signifies a diverse intake of essential nutrients crucial for managing fatty liver disease․ Each vibrant hue in fruits and vegetables often corresponds to different phytochemicals, antioxidants, vitamins, and minerals that collectively support liver function and reduce inflammation․ For instance, deep green leafy vegetables like spinach and kale provide chlorophyll and antioxidants, while red berries and bell peppers offer powerful anti-inflammatory compounds beneficial for liver health․
Orange and yellow foods, such as carrots, sweet potatoes, and citrus fruits, are packed with beta-carotenes and Vitamin C, which aid in detoxification and protect liver cells from damage․ Purple foods like blueberries and eggplant contain anthocyanins, known for their strong antioxidant properties․ Making a conscious effort to include a rainbow of produce in every meal—whether through a colorful salad, a vegetable-rich stir-fry, or a fruit smoothie—ensures a broader range of protective compounds․ This strategy not only makes eating more enjoyable but also provides comprehensive nutritional support to combat fat accumulation and promote overall liver wellness․

Making Your Own Seasonings
Creating your own seasoning blends is a crucial step in managing fatty liver disease, allowing you to bypass hidden sugars, excessive sodium, and unhealthy additives commonly found in store-bought mixes․ Commercial seasonings often contain monosodium glutamate (MSG), preservatives, and anti-caking agents detrimental to liver health․ By preparing your own, you gain complete control over every ingredient, ensuring only beneficial herbs and spices enhance your meals․
Focus on natural, anti-inflammatory spices known for their liver-protective qualities․ Turmeric, with its active compound curcumin, powerfully aids in reducing inflammation and oxidative stress․ Garlic powder, onion powder, ginger, oregano, basil, and rosemary are excellent choices, adding robust flavor without compromising your liver health․ These fresh or dried herbs not only boost taste but also contribute valuable antioxidants and phytonutrients․ This practice helps eliminate potential toxins, supporting liver detoxification and overall wellness for optimal disease management․

Foods to Avoid and Lifestyle Support
Avoid processed foods, high carbs, MSG, and vegetable/seed oils․ Essential lifestyle support includes daily exercise and ensuring 7-8 hours of quality sleep; critical for managing fatty liver disease․
Eliminating Processed Foods and High Carbs
A critical step in managing fatty liver disease is the rigorous elimination of processed foods and high-carbohydrate items from your diet․ Processed foods, often packed with hidden sugars, unhealthy fats, artificial ingredients, and excessive sodium, significantly contribute to liver fat accumulation and inflammation․ These items provide empty calories, thereby burdening the liver’s metabolic capacity․ Common examples include sugary drinks, fast food, packaged snacks, and refined baked goods․
Similarly, a high intake of refined carbohydrates like white bread, pasta, pastries, and sugary cereals exacerbates hepatic steatosis․ When consumed, these rapidly break down into glucose, causing detrimental spikes in blood sugar and insulin․ The liver then converts excess glucose into fat, directly contributing to fatty liver disease progression, especially in those with obesity and type 2 diabetes․ By consciously avoiding these dietary culprits, you significantly reduce the liver’s workload, decrease inflammation, and support its detoxification and regeneration․ This strategic dietary shift is paramount for fostering liver healing and overall health․

Limiting MSG and Vegetable/Seed Oils
For effective fatty liver management, it is crucial to carefully limit your intake of monosodium glutamate (MSG) and certain vegetable or seed oils․ MSG, a common flavor enhancer often found in processed foods, restaurant meals, and packaged snacks, has been linked to potential metabolic disturbances and inflammation․ Reducing its consumption can alleviate some of the burdens on a compromised liver and support healthier metabolic pathways․
Furthermore, a significant reduction in highly processed vegetable and seed oils, such as soybean, corn, sunflower, and canola oils, is strongly advised․ These oils are typically high in omega-6 polyunsaturated fatty acids, which, when consumed in excess relative to omega-3s, can promote systemic inflammation and oxidative stress within the liver․ This inflammatory environment can exacerbate liver damage and hinder recovery from hepatic steatosis․ Opting for healthier fat sources in moderation, like extra virgin olive oil or avocado oil, is a much better choice․ This conscious reduction in MSG and inflammatory oils plays a vital role in creating a liver-friendly dietary environment․
Importance of Daily Exercise
Incorporating daily exercise is a cornerstone of effective fatty liver disease management, extending beyond just dietary adjustments․ Regular physical activity plays a critical role in reducing the accumulation of fat in the liver, a primary characteristic of hepatic steatosis․ Engaging in consistent movement helps to burn calories, facilitate weight loss or maintenance, and improve overall metabolic health․
Exercise directly enhances insulin sensitivity, which is particularly beneficial for individuals with associated conditions like type 2 diabetes and obesity․ Improved insulin sensitivity means the body can utilize glucose more efficiently, reducing the amount stored as fat in the liver․ Furthermore, daily exercise contributes to a reduction in systemic inflammation and oxidative stress, both of which can exacerbate liver damage․ Even moderate activities, like brisk walking, cycling, or swimming, when performed consistently as part of your daily routine, can significantly contribute to liver health and help reverse the progression of fatty liver disease․ It’s a vital component of a comprehensive approach to combating this condition․
Achieving 7-8 Hours of Sleep
Achieving adequate sleep, specifically 7-8 hours per night, is a crucial, yet often overlooked, component in the holistic management of fatty liver disease․ As highlighted by experts like “The Liver Doc” or Dr․ Cyriac Abby, consistent quality sleep plays a significant role in supporting overall liver health and aiding in the reversal of hepatic steatosis․ Sleep deprivation can disrupt metabolic processes and hormonal balance, which are intrinsically linked to fat accumulation in the liver․
Lack of sufficient sleep can lead to increased insulin resistance, a key contributor to the development and progression of non-alcoholic fatty liver disease (NAFLD)․ Furthermore, poor sleep patterns can elevate levels of stress hormones, which may promote inflammation and the storage of fat within liver cells․ Prioritizing consistent, restorative sleep allows the body to effectively repair, regulate metabolism, and manage blood sugar levels, thereby creating a more favorable internal environment for liver recovery․ Integrating this essential lifestyle habit alongside dietary changes and exercise forms a powerful strategy against fatty liver disease․